

Ketosis
A Common Metabolic Disorder in Early Lactation Dairy Cows
Ketosis, or elevated ketones in the blood, can be physiological as long as cows are healthy. It is not a problem if the turnover of non-esterified fatty acids (NEFAs) is high, but NEFAs greater than 0.6 mmol/l after calving do increase probability of disease.
Ketosis can occur1:
- When energy intake is limiting ketosis from three to six weeks post calving
- From days three to 21 after calving associated to inability to adapt to NEB
Combination of intense adipose mobilization and a high glucose demand, both present in early lactation.
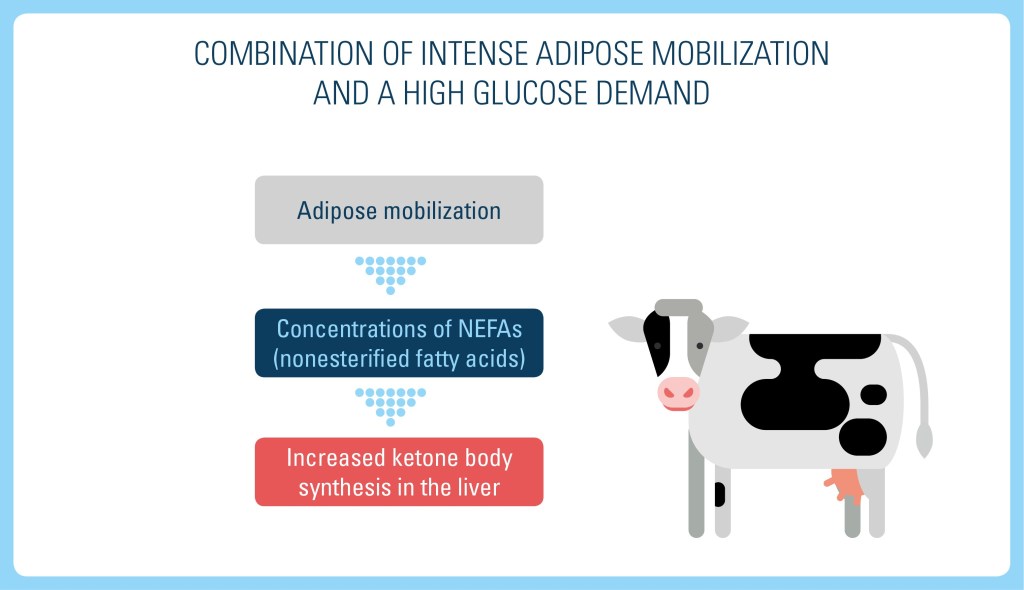
Ketosis in the immediate postpartum period (ketosis type II) is usually associated with fatty liver. Both are probably part of a spectrum of conditions associated with intense fat mobilization in cattle.
Ketosis occurring closer to peak milk production (ketosis type I) may be more closely associated with underfed cattle experiencing a metabolic shortage of gluconeogenic precursors than with excessive fat mobilization.
- Reduced feed intake (often refuse grain before forage)
- Reduced milk production
- Lethargy
- Slightly dehydrated
- In a minority of cases, CNS disturbances, incoordination and gait abnormalities
Clinical Diagnosis Is Based on Presence of Risk Factors, Clinical Signs and Ketone Bodies in Urine or Milk
Ketosis frequently occurs concurrently with other peripartum diseases such as:
- Displaced abomasum
- Retained fetal membranes
- Metritis
A fat-to-protein ratio (FPR) cut-off > 1.25 serves to diagnose subclinical ketosis (SCK), so not all cows would have to be checked if a herd has a systematic monitoring schedule for diagnosis of SCK2.
Cow-side tests for the presence of ketone bodies in urine or milk are critical for diagnosis. Dipstick tests are convenient, but those designed to detect acetoacetate or acetone in urine are not suitable for milk testing.
Handheld instruments designed to monitor ketone bodies in the blood of human diabetic patients are also available.
The gold standard ketosis test is blood β-hydroxybutyric acid (BHBA), the most accurate for herd monitoring, but cow-side ketosis tests are cheaper, require less labor and allow immediate results when compared to blood BHBA testing. One can do both urine and milk tests for ketosis.
Treatment options:
- Bolus IV administration of 500 mL of 50% dextrose solution
- Bolus glucose therapy generally results in rapid recovery, especially in type I ketosis. However, the effect is frequently transient, and relapses are common.
- Glucocorticoids, including dexamethasone or isoflupredone acetate at 5-20 mg/dose, IM
- Propylene glycol administered orally (250-400 g/dose [8-14 oz]) once per day acts as a glucose precursor
Type II ketosis frequently are more refractory to therapy type I:
- Continuous IV glucose infusion and tube feeding
Nutritional management:
- Modifying diets of late lactation cows to increase the energy supply from digestible fiber and reduce the energy supply from starch
- Maintaining and promoting feed intake
- Administering some feed additives such as niacin, calcium propionate, sodium propionate, propylene glycol and rumen-protected choline. To be effective, they should be fed in the last two to three weeks of gestation as well as during the period of ketosis susceptibility.
- Amaral-Phillips, D.M. 2015. Monthly Webinar Review: Treatments for Dairy Cows with Ketosis. Cooperation Extension Service. University of Kentucky.
- Jenkins, N.T., Peña, G., Risco, C., Barbosa, C.C., Vieira-Neto, A., Galvão, K.N. 2015. Utility of inline milk fat and protein ratio to diagnose subclinical ketosis and to assign propylene glycol treatment in lactating dairy cows. The Canadian Veterinary Journal, 56(8), 850–854.

